Dental Diode Laser vs CO₂ Laser vs Er,Cr:YSGG Laser: Which Equipment Is Best for Your Dental Practice?
Dental lasers have significantly transformed global dental practice through improved precision, minimal invasiveness, and enhanced patient comfort. From diode and CO₂ lasers to water and erbium lasers, each type has distinct physical characteristics, clinical uses, and operational considerations. This article explores the types, mechanisms, safety profiles, indications, contraindications, market landscape, and future directions of dental lasers to support informed decision-making for clinicians worldwide.
Characteristics of Diode Laser | CO₂ Laser | Er,Cr:YSGG Laser
CO₂ Laser (e.g., Solea)
Wavelength: 9300–10,600 nm
Mechanism: Absorption by water; vaporizes tissue with strong hemostatic effect
Clinical Uses: Soft-tissue surgeries (gingivectomy, frenectomy), some hard tissue applications
Advantages: High precision, bloodless field, minimal postoperative swelling
Limitations: Thermal risk to adjacent tissues, bulky equipment, high cost
Safety/Efficacy: High efficacy in soft-tissue ablation, but requires expertise to avoid overheating
Diode Laser (e.g., Pioon S3 Triple-Wavelenth)
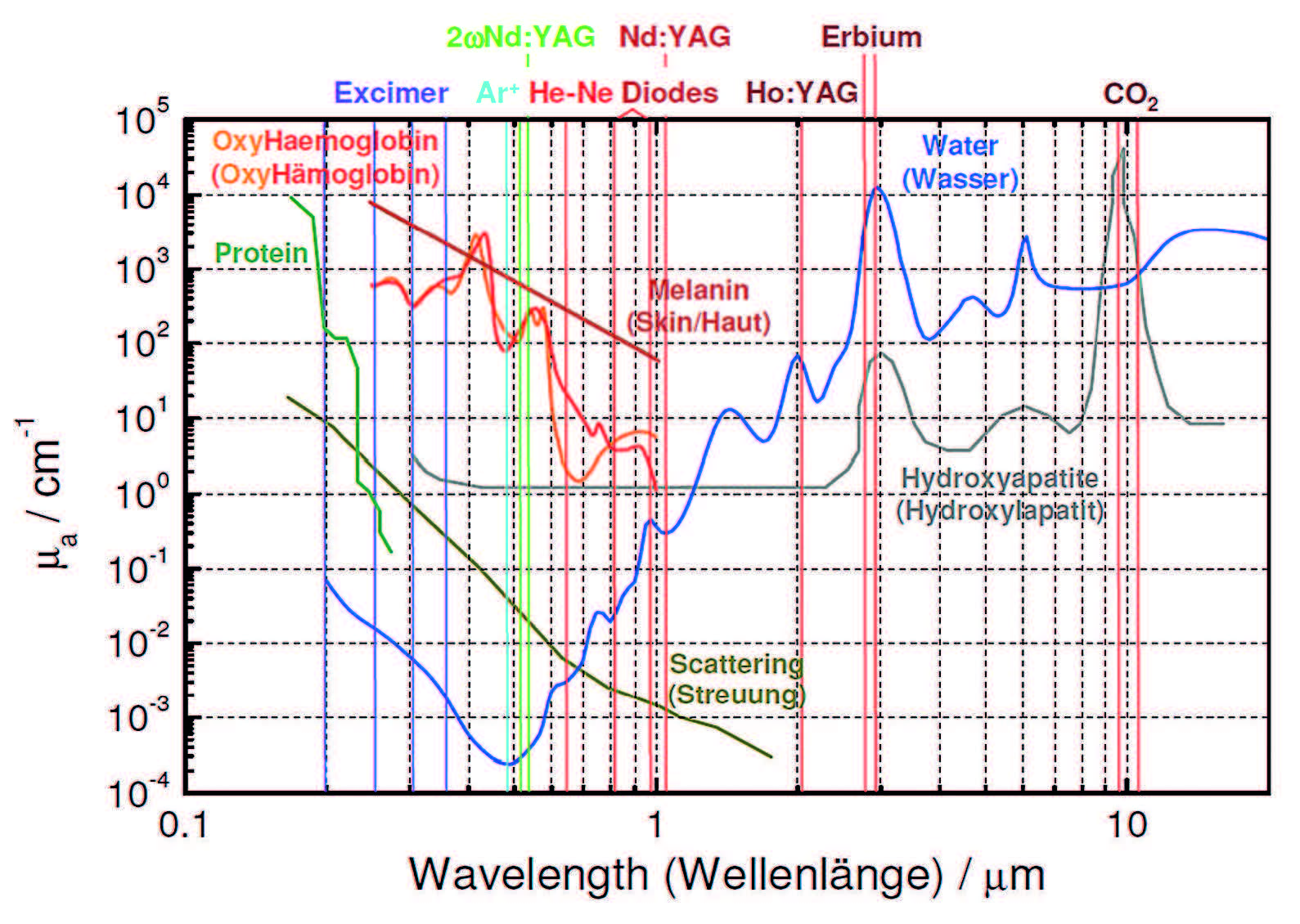
Wavelength: 450–980 nm
Mechanism: Photothermal and biostimulatory effects; absorbed by melanin and hemoglobin
Clinical Uses: Periodontal therapy, soft-tissue surgery, low-level laser therapy (LLLT), aesthetics
Advantages: Compact, cost-effective, easy to use, extensive indications (8 major clinical areas, 57 treatment protocols)
Limitations: Ineffective on hard tissues, limited penetration depth
Safety/Efficacy: Safe for general practice with proper settings; excellent for soft-tissue healing and inflammation reduction
Case Highlight: 450nm Blue Diode Laser for Gum Depigmentation
The 450nm blue laser strongly absorbs hemoglobin, enabling precise removal of gum pigmentation with minimal bleeding, fast recovery, and low discomfort—ideal for children or anxious patients.
Case Source: laserdentistry.org

Er,Cr:YSGG (Water Laser – e.g., Biolase Waterlase)
Wavelength: 2780 nm
Mechanism: Hydrokinetic energy via water excitation
Clinical Uses: Caries removal, crown prep, root canal disinfection, soft-tissue incisions
Advantages: Minimally invasive, reduced anesthesia, low thermal damage
Limitations: High cost, requires steep learning curve and consumables
Safety/Efficacy: High safety and efficacy in both soft and hard tissues; patient-friendly
Er:YAG Laser (e.g., Fotona LightWalker)
Wavelength: 2940 nm
Mechanism: Micro-explosive ablation via high water absorption
Clinical Uses: Cavity prep, enamel etching, implant decontamination
Advantages: Clean hard-tissue cutting, minimal thermal side effects
Limitations: Less effective in soft-tissue hemostasis, cost-intensive
Safety/Efficacy: Highly effective for enamel and dentin; requires precise control
Differences and Characteristics Of Diode Laser | CO₂ Laser | Waterlase
| Feature | CO₂ Laser | Diode Laser | Waterlase |
| Wavelength | 10.6 µm (10600 nm), newer 9300 nm/9600 nm |
450–980 nm |
2780 nm (Er,Cr:YSGG) or 2940 nm (Er:YAG) |
| Absorption | High water absorption, ideal for wet tissues (gums, teeth) | Pigment absorption (hemoglobin, melanin), suits vascular tissues |
Water and hydroxyapatite, suits soft/ hard tissues |
| Cutting Ability | Deep, efficient cutting for large soft tissue surgeries |
Shallow, gentle cutting for minor procedures |
Precise cutting for soft/hard tissues, hydrokinetic action |
| Hard Tissue | Newer 9300 nm/9600 nm for enamel/dentin |
Not for hard tissue | For enamel, dentin, bone |
| Hemostasis | Excellent, rapid vessel coagulation |
Good, slightly less effective | Moderate, may have minor bleeding |
| Pain Management | Indirect via reduced trauma | Direct via LLLT for pain relief | Minimal pain, often no anesthesia needed |
| Penetration | Shallow, surface-focused | Deep, risks deeper tissue damage | Moderate, water spray controls depth |
| Equipment |
Large, costly, complex maintenance ($30,000–$80,000) |
Compact, affordable, simple ($8,000–$20,000) |
Medium-sized, costly, requires water system ($40,000–$85,000) |
| Comfort | Fast but may need anesthesia | Mild, often no anesthesia | Mild, minimal anesthesia |
| Healing | Larger thermal damage, slower healing |
Minimal thermal damage, fast healing |
Least thermal damage, fastest healing |
Clinical Scenarios
When to Choose a CO₂ Laser:
Major Surgeries: For cases like severe gum overgrowth or removal of large oral tumors, a CO₂ laser cuts quickly and causes minimal bleeding.
Hard Tissue (Advanced Use): Newer CO₂ lasers (like 9300 nm) are effective for cavity prevention and treating dentin hypersensitivity.
Fast Bleeding Control: After tooth extractions, CO₂ lasers help stop bleeding quickly and disinfect the area.
Example: A patient has gum tissue covering a wisdom tooth. The CO₂ laser cleanly removes it in seconds, and healing only takes a few days.
When to Choose a Diode Laser:
Minor Procedures: Ideal for small gum reshaping or treating minor ulcers. Diode lasers are gentle and often painless.
Pain Relief: After surgery, low-level laser therapy (LLLT) can reduce gum swelling and pain effectively.
Teeth Whitening: When used with whitening gels, diode lasers are simple to operate and widely adopted in clinics.
Example: A patient with mild periodontitis receives diode laser treatment to kill bacteria and promote gum healing. It's quick and comfortable.
Mainstream blue triple-wavelength dental lasers, such as the Pioon S3 soft tissue laser that covers 8 major clinical areas and 57 treatment protocols, delivering exceptional versatility and broad clinical value

When to Choose Waterlase:
Hard Tissue Work: Perfect for treating cavities or smoothing tooth surfaces. Waterlase replaces drills, making treatment quiet and pain-free.
Combined Soft & Hard Tissue Surgery: During implant procedures, Waterlase can shape both the bone and gums in one go.
For Anxious Patients: Waterlase usually doesn’t require anesthesia, making it ideal for children or patients afraid of dental drills.
Example: A child has a cavity. Waterlase gently "sprays" away the decay with almost no pain, giving parents peace of mind.
Limitations and Notes
CO2 Laser: Hard tissue applications (9300 nm/9600 nm) are relatively new, with fewer long-term clinical studies compared to soft tissue uses. Most evidence is from controlled trials (e.g., Effects of 9,300 nm CO2 Laser).
Diode Laser: Limited to soft tissue, with no peer-reviewed studies supporting hard tissue use. LLLT benefits are well-documented but vary by patient
Waterlase: Extensive clinical data support its efficacy, but weaker hemostasis is noted in reviews. Equipment costs and water system maintenance are practical barriers.
Future Outlook: Opportunities and Challenges
As the dental laser market continues to evolve, several trends and challenges are shaping its future.
Trends include the miniaturization of laser systems, the integration of AI for smarter energy delivery, software-guided treatment protocols, and the adoption of wireless foot pedals for enhanced ergonomics.
Challenges remain in terms of cost barriers for high-end systems, extensive training requirements, and regulatory inconsistencies between regions—particularly concerning hygienist usage rights.
Market Growth: According to Fortune Business Insights, the global dental lasers market size was valued at USD 245.5 million in 2022 and is projected to grow at a CAGR of 5.4% to reach USD 371.8 million by 2030. While North America leads, the Asia-Pacific region is rapidly catching up due to growing dental awareness, government oral health initiatives, and increased investment in private dental care.
Curious about the ROI of dental lasers and how they can give your clinic a competitive edge? Dive into this article to discover how laser technology can elevate your practice and profitability.
Conclusion
Dental lasers continue to evolve, bridging advanced technology with clinical demand. Diode lasers remain the go-to for general and soft-tissue applications, offering a balance of affordability and effectiveness. For full-spectrum practices, combining CO₂ or erbium lasers with diode systems allows comprehensive care.
Ultimately, successful laser adoption depends on clinical need, budget, patient volume, and proper training. As innovation and education expand, dental lasers will become a standard part of modern dental workflows worldwide.